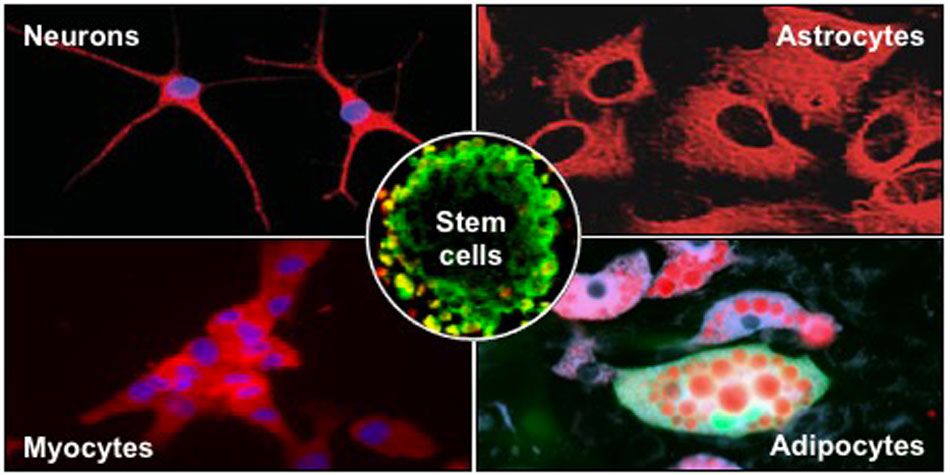

The olfactory mucosa is home of a permanent neurogenesis. Our team was the first to identify and characterise the adult ecto-mesenchymal stem cells residing in the human nasal olfactory lamina propria. These easily accessible cells, located in a nervous tissue, allowed us to find new candidate genes in brain pathologies. We successfully identified specific risk factors for Parkinson’s disease, schizophrenia and bipolar disorders. We also demonstrated a misexpression of molybdenum enzymes and a perturbed purine metabolism in autistic patients. Currently, we perform frontline sequencing techniques (genome, transcriptome, metabolome) to unveil common phenotypes in autism spectrum disorders.
We also used olfactory stem cells to repair central and peripheral nervous systems. We transplanted undifferentiated stem cells in animal models of amnesia and Parkinson’s disease. In both cases, grafted cells differentiated and improved the host behaviour, namely learning abilities or locomotion. We also devised a protocol enabling an in vitro transdifferentiation into dopaminergic neurons. In parallel, we conducted a series of experiments based on the grafting of olfactory stem cells in injured peripheral nerves. Two pilot clinical trials, based on the autologous transplantation of olfactory stem cells in patients with a lesioned facial or hand nerve, are currently implemented.
We also develop an innovative therapy to repair pepheral nerves using the Extracellular Vesicles produced by the olfactory stem cells. Indeed, the therapeutic benefit of stem cells is primarily related to the trophic and immune factors they secrete, notably, via their extracellular vesicles.
| Attachment | Size |
|---|---|
| 124.21 KB | |
| 870.58 KB |